What care teams had already observed in practice is now independently confirmed through a public-sector evaluation: once Nobi is installed in care homes, fall-related incidents are detected earlier, serious outcomes decrease, and escalation to emergency services drops, with direct consequences for hospital utilisation and system-level costs.
Published by Suffolk & North East Essex Integrated Care Board (SNEE ICB), the evaluation examined real-world outcomes across seven care homes (87 rooms) in Suffolk. The study was delivered under the NHS Digitising Social Care Programme, using NHS funding allocated to the ICB to assess the impact of digital care technology in frontline settings.
Implementation was delivered in partnership with Porters Care, with support from Suffolk County Council and participating care providers.
Results at a glance
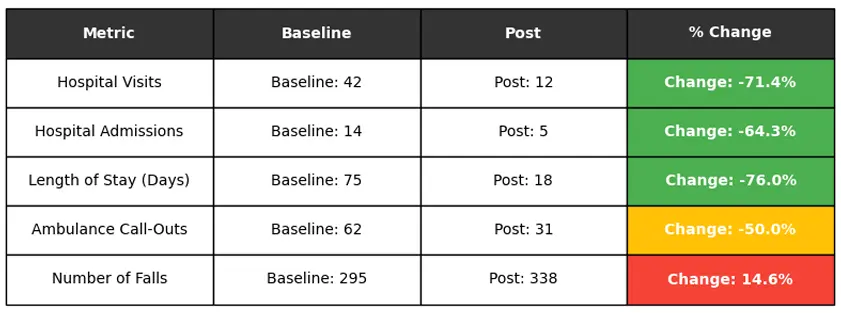
Across the seven homes, SNEE ICB reports:
- fewer fall-related hospital visits, admissions and ambulance callouts
- dramatically shorter hospital stay when admission occurs
- more complete incident visibility (falls recorded, fewer escalations)
The ICB’s interpretation is explicit: these outcomes indicate earlier detection, faster response times and safer on-site management of falls, no delays or avoided escalations.
The strongest signal sits in the combination: fewer fall-related admissions and a much shorter length of stay. This is what drives the biggest system impact (acute capacity pressure and downstream costs).
Why recorded falls increased, and why that’s a positive signal
The evaluation directly addresses the observed increase in recorded falls. According to the ICB, this reflects improved detection of previously unwitnessed or self-resolved incidents, rather than an increase in fall risk.
At the same time, ambulance callouts and hospital admissions declined, indicating greater visibility with reduced unnecessary escalations.
What changed in day-to-day practice
Alongside the numbers, the evaluation documents consistently demonstrate qualitative change once Nobi is embedded into daily work.
Across homes, staff report:
- higher confidence (especially on night shifts);
- less guesswork and faster triage after incidents;
- stronger documentation supporting regulatory confidence;
- clear cultural adoption (described as “embedded into daily practice”).
Families describe the same shift:
- clearer explanations when incidents occur;
- reduced guilt around care placement;
- increased peace of mind.
There was at least one documented case where Nobi influenced the choice of senior living community.
Taken together: better fall insight strengthens judgement on the care floor, and builds trust with families.
System-level value
The report’s cost analysis is grounded in the clinical reality above: fewer admissions and shorter stays reduce pressure on acute services and lower system costs.
Using conservative NHS reference costs, SNEE ICB estimates:
 Avoided fall-related emergency-care costs
Avoided fall-related emergency-care costs
over six months
 Avoided costs
Avoided costs
over three years
 ROI
ROI
over three years
 Payback
Payback
The report explicitly notes these figures represent system-level value, not optimistic vendor assumptions or provider-specific savings.
Beyond falls: scaling into predictive care
While falls were the primary focus, the evaluation also documents real-world use of Nobi data beyond immediate fall response — supporting earlier, more proactive care decisions.
Including:
- sleep disruption patterns supporting earlier detection of UTIs;
- behavioural health monitoring;
- epilepsy pattern recognition;
- self-harm risk monitoring;
- mental-health and medication reviews.
These applications are described as current practice, not future potential. Taken together, they frame Nobi as care infrastructure, supporting predictive and preventative care, not a single-use fall solution.
Raising the standard for care
In its conclusions, Suffolk & North East Essex ICB is explicit. In the context of the NHS ten-year plan and the accelerated shift from analogue to digital care, the evaluation states that smart fall-prevention and monitoring technologies should not be treated as optional innovation.
Instead, the evaluation calls for smart monitoring to be progressively normalised within market-shaping guidance, provider digital maturity pathways and falls prevention strategies and positioned as a recommended standard within commissioning expectations for older people’s care and supported living.
For Nobi, this conclusion directly reflects how we design and position our technology: not as an add-on, but as care infrastructure that belongs in the standard of care.
Wondering what this research means for your care environment?
Read a preview of the ICB-study here.
Please provide your details to receive the full report, or contact us for further information.